The Salvation Army in Nebraska helps people experiencing homelessness to stabilize following psychiatric crises.
By Jared McKiernan –
Lonnie Hennings didn’t realize it, but he was suffering from severe mental illness. Then, four months ago he hit a threshold.
“I had some thoughts of not wanting to live anymore and just…I was tired of being tired,” Hennings said. “Bills were piling up, I lost my apartment, I lost my job––I lost everything. I was homeless. If you were to talk to me on June 2, which was not too long ago, I had nothing.”
He checked into a mental hospital, where he was diagnosed with bipolar disorder and began to work toward stability.

Dr. Carole Lieberman, clinical faculty member at the University of California, Los Angeles Neuropsychiatric Institute, defines stability as the point when the patient begins to get insight into his or her problems, has no acute symptoms, is not homicidal or suicidal, is on a medication regime that is working well, has a follow-up appointment with a psychiatrist and understands the importance of continuing therapy and medication.
Yet, the initial stabilization period in mental hospitals may not suffice for many, Lieberman said. Patients often need support beyond their hospital stays to prevent future psychiatric crises, particularly if they are homeless.
“Hospitals are too quick to discharge patients these days because of rising cost, especially if the patient has no insurance to pay for it,” Lieberman said. “Therefore, the more supervision and support that a person can have after hospitalization––such as in halfway houses, or day treatment or respite care––is invaluable to solidify their stabilization. Stabilization takes a long time.”
Hennings said he needed extra time to put himself “back together” after his crisis so he entered The Salvation Army’s Mental Health Respite (MHR) facility in Omaha, Neb.
MHR is a 28-day residential program that can accommodate up to 16 homeless, mentally ill adults 19 or older who need to further stabilize following a hospitalization––Nebraska’s only program of its kind, according to Program Director Darsey Zwiener. Launched in 1993, MHR offers independent living skills training such as hygiene, cleaning, cooking and money management as well as housing and employment resources. About 75 percent of referrals are for individuals who have been inpatient for psychiatric reasons.
“Our population is at very high risk for relapsing mental health,” Zwiener said. “Generally they’re homeless, so we help them figure out what resources they could afford in the community. Have they applied? Are they eligible? Right now I just see a lot of individuals going out of a hospitalization inpatient and going back to an environment where there is no support, no accountability and no assistance with getting things set up for them so they’re thrown back into a chaotic environment.”
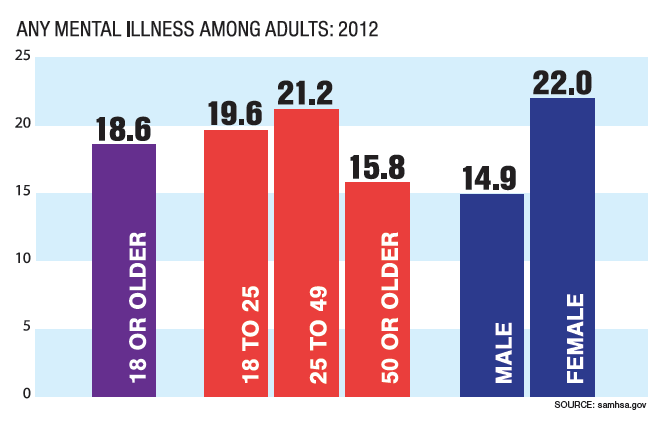
According to the Substance Abuse and Mental Health Services Administration (SAMHSA), up to 30 percent of the homeless population in the United States suffer from some form of mental illness. They’re gripped by bipolar disorder, schizophrenia or severe depression––all manageable with the proper intervention but agonizing if left untreated.
Though SAMHSA lists mental illness as a structural cause of homelessness, becoming homeless can actually intensify the symptoms of a mental illness and even trigger a psychiatric crisis, said Dr. Stacey Lambert, chair of the Department of Clinical Psychology at the Massachusetts School of Professional Psychology.
 “There are social factors that contribute to the decompensation of the mental illness,” Lambert said. “For example, if someone loses their job or loses their housing, that might kick off a depression or a psychotic episode. You have to have the biological vulnerability for the mental illness. You don’t get a psychotic disorder necessarily just from losing your job but if you have the genetic predisposition and the stressor acts on the biological vulnerability, that can cause the initial emergence as well as the repeated episodes of the illness.”
“There are social factors that contribute to the decompensation of the mental illness,” Lambert said. “For example, if someone loses their job or loses their housing, that might kick off a depression or a psychotic episode. You have to have the biological vulnerability for the mental illness. You don’t get a psychotic disorder necessarily just from losing your job but if you have the genetic predisposition and the stressor acts on the biological vulnerability, that can cause the initial emergence as well as the repeated episodes of the illness.”
Therefore, if patients do not secure housing and employment while stabilizing, they remain more vulnerable to future psychiatric crises, Lambert said.
Lianne Reed, MHR case manager, noted that even 28 additional days can become a tight window for helping clients return to relative independence.
“Some of the clients get comfortable here but getting a client into housing can take longer than 28 days so we try to find backup plans and things that are going to be helpful for them,” Reed said. “There’s a chance that they’re not going to get their actual housing goal met.”
In that case, MHR may offer clients extensions based on whether they are “stable enough to where they can work on their goals in their community,” she said.
Hennings capitalized on his stay at MHR, securing both a job with Goodwill Industries and his own apartment.
His bipolar disorder is still active but it is being monitored.
He said he eventually wants to return to California to sell advertising like he used to, but not just yet.
“I don’t want to just tell people I’m grateful with words, I want to show them and that’s huge for me and my recovery,” he said. “I want to be in that role [of peer support] back here, even if it’s part time.
“At the end of the day if you utilize the resources they give you at The Salvation Army there’s no reason you can’t be successful,” he said. “It does take work. It’s nothing that happens overnight. You’ve got to apply yourself.”